Hidradenitis Suppurativa (HS)
Hidradenitis Suppurativa (HS), also known as acne inversa, is a chronic inflammatory skin condition that primarily affects specific areas of the body such as the axillae, groin, perianal, perineal, and inframammary locations. It is characterized by persistent or recurrent boil-like nodules and abscesses that culminate in a purulent discharge, sinuses, and scarring.
Etiology and Pathophysiology
Hidradenitis suppurativa (HS) is a complex skin condition with multiple causes. It is influenced by genetic, environmental, and behavioral factors. Genetic factors include a mutation in the gamma-secretase Notch signaling pathway found in some affected families. Environmental factors like obesity and smoking, as well as hormonal influences, contribute to the development of HS. The condition involves blockage of hair follicles, abnormal skin bacteria, inflammation, and damage to glands and ducts. The exact cause of HS is unknown, but it is likely a combination of genetic predisposition, hormonal changes, immune system dysfunction, and external factors that contribute to its development and severity.
Distinctive Features
HS typically manifests as painful nodules or boils in the affected areas, progressing to form abscesses and interconnected sinus tracts. These lesions have a tendency to recur and can persist for weeks or even months, resulting in the formation of scars and thickening of the skin. HS significantly impacts a person’s quality of life, causing persistent pain, discomfort, and emotional distress.
Clinically, HS is characterized by a range of specific features, including open double-headed comedones, painful firm papules and nodules, pustules, fluctuant pseudocysts, and abscesses. Additionally, the disease is marked by draining sinuses that link the inflammatory lesions, and it can lead to the development of hypertrophic and atrophic scars.
Diagnosis
Diagnosing HS can be challenging due to its variable presentation and similarities to other skin conditions. Clinical diagnosis requires recognition of the morphology (deep, inflamed, painful nodules, sinus tracts, scars), the location (intertriginous areas, apocrine gland-containing areas), and the chronicity of the disease process (prolonged course with periods of activity and remission).
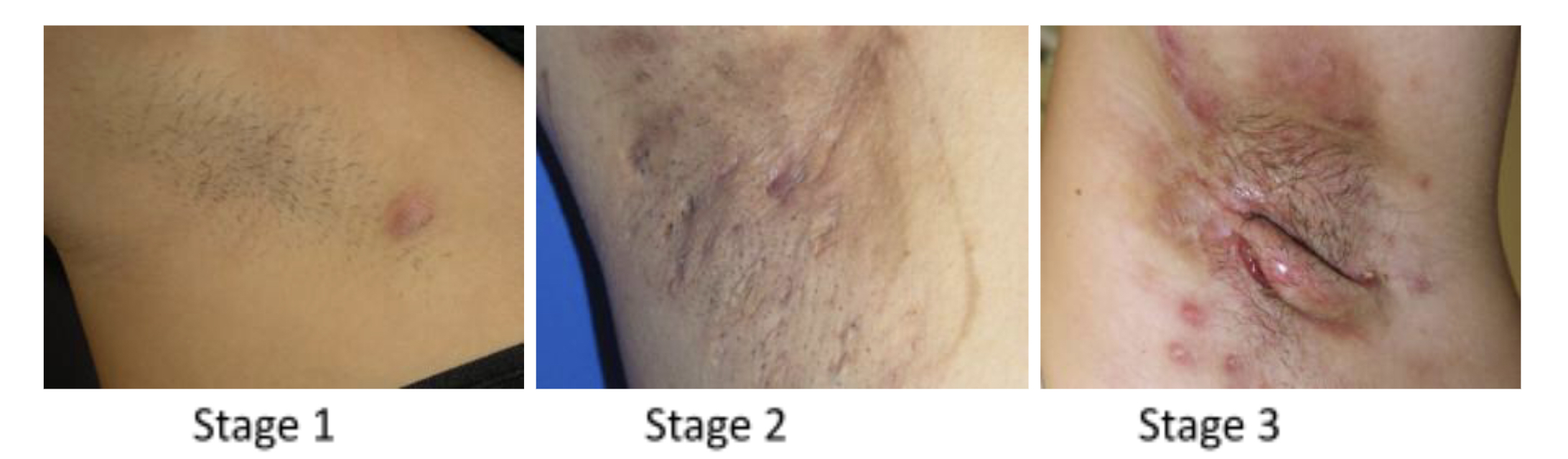
The Hurley staging system is commonly used to classify the severity of HS:
Stage I: Single or multiple abscesses without sinus tracts or scarring.
Stage II: Recurrent abscesses with sinus tracts and scarring in two or more areas.
Stage III: Multiple interconnected sinus tracts and abscesses involving larger areas, with significant scarring.
In some cases, additional tests, such as swabs to rule out infection or biopsies for histopathological examination, may be performed to confirm the diagnosis or exclude other conditions.
Management:
Treatment options for hidradenitis suppurativa (HS) encompass various approaches based on the severity of the condition. These include:
- Lifestyle Modifications: Patients are advised to maintain good hygiene, avoid tight-fitting clothing, quit smoking, and manage weight if overweight or obese. These lifestyle modifications can help reduce friction, sweating, and inflammation in the affected areas.
- Topical Treatments: In milder cases, topical treatments such as antibacterial washes, topical antibiotics (e.g., clindamycin phosphate 1% with benzoyl peroxide), and anti-inflammatory creams can be effective. These interventions aim to reduce bacterial colonization and inflammation.
- Systemic Medications: For moderate to severe HS, systemic medications may be prescribed. Antibiotics like tetracycline or clindamycin can be administered to suppress bacterial growth. Anti-androgen medications like spironolactone may be considered for women with hormonal influences. Biologic therapies, such as TNF-alpha inhibitors like adalimumab, have shown promise in reducing inflammation and disease activity.
- Surgical Interventions: In cases where medical therapy proves insufficient, surgical interventions may be necessary. These can include incision and drainage of abscesses, excision of affected tissue, and laser therapy to manage persistent or recurrent lesions.
Written by
Deemah AlHuraish, medical student
Revised by
Maee Barakeh, medical student
References
DermNet
NCBI