Steven-Johnson Syndrome (SJS) and Toxic epidermal necrolysis (TEN)
Introduction:
SJS and TEN are rare, acute, and potentially fatal reactions affecting the skin and the mucous membrane. The evidence suggests that both SJS and TEN result from a defect in detoxifying drug metabolites, inducing immune responses. Moreover, Interaction between drug metabolites and immune cells causes extensive keratinocyte cell death via apoptosis, leading to dermo-epidermal junction separation, causing detachment of the skin and the mucous membrane.
Etiology:
Medications are the leading offending cause of SJS and TEN, where they have been reported in more than 95% of TEN cases. The most common drugs that cause SJS and TEN are allopurinol, antibiotics (e.g. Sulfonamides), nonsteroidal anti-inflammatory drugs, and anticonvulsants (e.g. Phenytoin). SJS and TEN usually happen between 7-21 days after initiation of causative medications, while some medications (e.g. Anticonvulsants) may take up to 2 months to develop SJS and TEN. However, they occasionally occur as a result of infection or immunization.
Classification:
Steven-Johnson Syndrome: 10% body surface area (BSA) detachment
Overlapping SJS/TEN: 10-30% of the BSA detachment
Toxic epidermal necrolysis: 30% of the BSA detachment
Clinical Presentation:
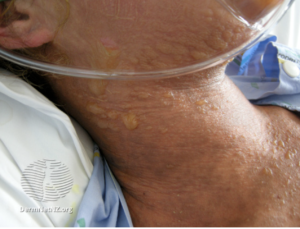
Initially, fever, conjunctivitis, and body aches can precede mucocutaneous presentation by 1-3 days. The cutaneous manifestation usually starts as sudden, tender/painful erythema of the skin. It first appears on the trunk, spreading to the neck, face, and proximal upper extremities. Skin lesions in SJS and TEN can present as purpuric macules, diffuse erythema, targetoid lesion, and/or flaccid blisters. In addition, Mucosal erythema and erosions are present in more than 90% of patients.
Diagnosis:
SJS and TEN are diagnosed by history and clinical presentation with a histopathologic evaluation of skin lesion.
Management:
To have optimal management of SJS and TEN requires making the diagnosis as soon as possible, immediate identification and cessation of the offending drug, and supportive care. Furthermore, SJS and TEN need a multidisciplinary team that includes dermatology, internal medicine, ophthalmology, and plastic surgery.
- Supportive management includes admission to intensive care or burns unit, daily wound and eye care, paraffin sheet, and high protein soft diet. In addition to, fluid replacement, mucosal hydration, and pain management should be initiated once a diagnosis is made.
- Choices of medical treatment in SJS and TEN includes:
1. Cyclosporine (3-5 m/kg/day for 7-14 days)
2. IVIG (3-4 g/kg total dose over 3–4 days)
3. Single-dose etanercept 50 mg subcutaneous or infliximab IV once
4. Plasmapheresis
5. The use of steroids is controversial, only indicated within the first 72 hours.
Mortality and prognosis:
The course of SJS and TEN is unpredictable. Therefore, the mortality should be assessed and recorded at admission within 72 hours using SCORTEN score, a prognostic scoring system for predicting mortality in SJS and TEN. Furthermore, the leading causes of mortality in SJS and TEN are sepsis, renal failure, and/or massive water loss with electrolytes disturbance. Finally, complete skin healing of detached skin usually takes 3-4 weeks.
Written by: Dr. Ahmed Almutairi, dermatology resident.
Reference:
Bolognia 4th edition